Introduction
Hypertension is a real public health problem, considered a silent killer and a main cause of cardiovascular morbidity and mortality. Its complications are serious, causing more than 9.4 million deaths per year in the world. Nevertheless, national data concerning this illness in the south of Tunisia are scarce or even inexistent. A thorough meta-analysis published in 2017, including 1,479 studies and over 19 million adults, estimated the global prevalence of hypertension in 2015 at 1.13 billion, whereas it was 529 million according to the same meta-analysis. In Tunisia, the prevalence of hypertension is around 28–35%. The high level of prevalence of hypertension is underpinned by an increasingly ageing population and a worsening rate of obesity, which is on the rise not only in developing but also in developed countries. In some communities, excessive salt consumption also constitutes a substantial risk. Furthermore, the lack of awareness and access to healthcare services in certain regions contributes to the high prevalence of hypertension. Additionally, genetic factors and a family history of hypertension can also play a role in the increased risk within certain populations.
1. Purpose and method
1.1. Purpose
This study aims to determine the epidemiological, clinical, and therapeutic profiles of hypertensive patients in southern Tunisia, to assess the prevalence of different stages of hypertension and corresponding modifiable and non-modifiable risk factors among patients in Medenine city in southern Tunisia, to determine the types of medication used by hypertensive patients, and to assess the level of blood pressure control in this population.
1.2. Method
We conducted a descriptive, monocentric, observational study involving 1093 hypertensive patients followed up at the outpatient cardiology department of Medenine hospital in the southern Tunisian population. The study was carried out between April 15, 2019, and June 19, 2019, over a period of two months. The interview served to collect the patient’s medical history, confirm hypertensive status and duration of evolution (length of time), provide follow-up to control blood pressure, assess patient adherence to treatment, determine the coexistence of other associated cardiovascular risk factors such as smoking, a sedentary lifestyle, obesity, and diabetes, and collect documentation testifying to a previous investigation, particularly a cardiac ultrasound report. Additionally, the interview aimed to evaluate the patient’s understanding of their condition and educate them about lifestyle modifications that can help manage hypertension. It also sought to gather information about any family history of cardiovascular diseases to assess the patient’s genetic predisposition.
The blood pressure measurement method involves the simultaneous use of a sphygmomanometer and a stethoscope. The BP measurement protocol complies with the conditions laid down by the French Hypertension Society. These conditions include ensuring that the patient is in a seated position with their arm supported at heart level. Additionally, the sphygmomanometer should be properly calibrated, and the stethoscope should be placed over the brachial artery to accurately detect blood flow sounds. Data were entered and analyzed using IBM SPSS Statistics 22 and Excel 2016.
2. Results
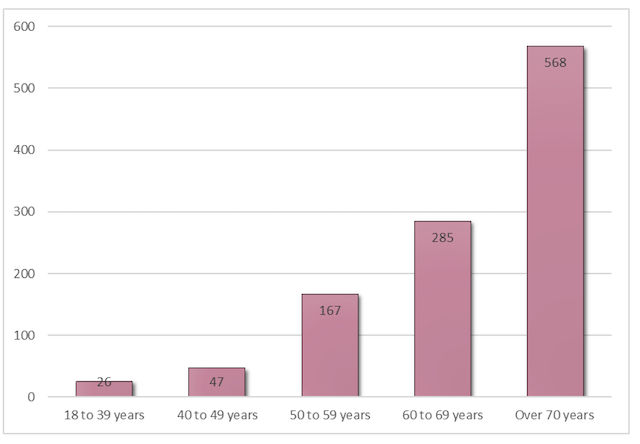
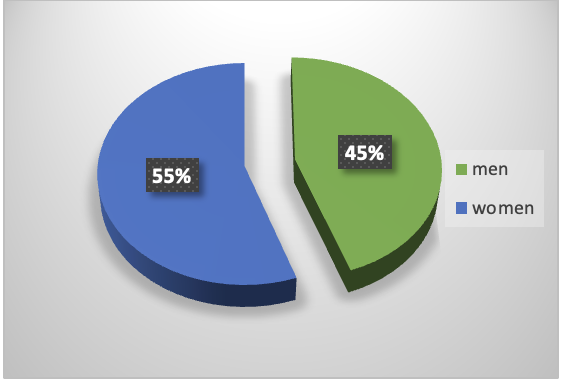
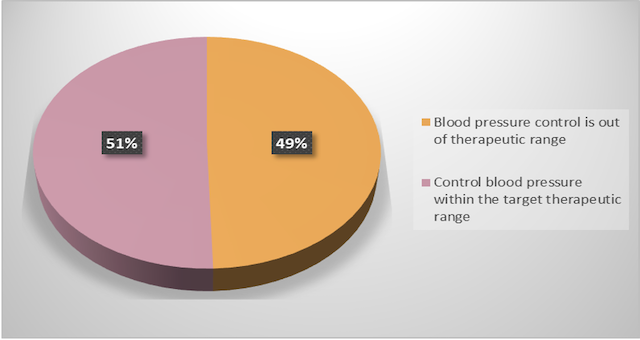
We included a total of 1093 patients with a mean age of 69 years (standard deviation 13.75) and a sex ratio of 0.67. Patients who were on antihypertensive treatment represented 47.8% of the population. Diabetes was the most frequent comorbidity (46.2%; n=505). Grade 1 hypertension accounted for 28.2%. The visceral complications of hypertension were dominated by cardiac involvement, particularly coronary artery disease, which was noted in 40.4% of patients, myocardial hypertrophy in 19.1%, and atrial fibrillation in 11.3%. Monotherapy was prescribed in 32.4% of patients and dual therapy in 10.8%. The angiotensin-converting enzyme inhibitor class was the most prescribed (33.4% of patients). The blood pressure target was achieved in half of the patients (50.5%).
3. Discussion
Diseases of the circulatory system ranked first in Tunisia in terms of mortality (25.8%) in 2017, according to the national statistics report on causes of death drawn up by the National Institute of Health. The TAHINA study, a cross-sectional investigation carried out between 2004 and 2005 on a population of 8007 individuals aged between 35 and 74, revealed a prevalence of hypertension of 30.6%. In southern Tunisia, and particularly in Medenine, the epidemiological profile of this clinical entity is still insufficiently documented. During the period from April 15, 2019, to May 15, 2019, data were collected on 1093 hypertensive patients aged 60 and over who were followed up in the outpatient department of the cardiology service of the regional hospital of Médenine. Although the proposed figure appears to be significant, it is, in fact, an underestimate given the many hypertensive patients who refrain from consulting a doctor due to various reasons such as lack of awareness, financial constraints, or fear of medical procedures. Additionally, cultural beliefs and traditional remedies may also contribute to the underreporting of hypertension cases in the region. The study sample had a female predominance with a male-to-female sex ratio of 0.67. This result is consistent with the THES national survey conducted in Tunisia in 2016 among 9,212 individuals aged 15 and over, which showed that the prevalence of hypertension is significantly higher in women than in men (30.8% vs. 26.5%; p <10-3). This could be due to the high representation rate of women in Tunisian society, which reached 50.41% of the population compared to 49.6% of men in 2020, according to the United Nations (UN). J. Martinoni also observed a male-to-female ratio of 0.37. The prevalence of hypertension is higher among women than men in sub-Saharan Africa (36.3%) and lower than men in high-income countries, with an estimated prevalence of 25.3%. The reasons for these disparities in the prevalence of hypertension between regions are not clearly determined and are probably influenced by differences in the prevalence of risk factors such as an unhealthy diet, a lack of physical activity, and obesity.
The majority of hypertensive patients in this study had moderately high blood pressure. Grade I hypertension (28.2%) was the most common, while severe grade III hypertension was the least common, with only 66 cases (6%). According to KONE S., 520 patients had slightly elevated blood pressure, accounting for 37.4% of the population, and 418 cases of severe hypertension, representing 29.86%.
A significant proportion of this population (44.6%) had previously known hypertension dating back 10 to 15 years. 65.2% of the patients studied were lost to follow-up, and 52.2% were not receiving any antihypertensive treatment. This phenomenon can be explained by a number of factors, including the lack of financial resources to purchase medication and the low level of education of the majority of patients, all of which are linked to a view of chronic disease that is only a cause for concern when it becomes very disabling. For example, in rural communities with limited access to healthcare, many patients have been living with hypertension for over a decade. Due to their low income and lack of education, they struggle to afford regular medication and do not fully understand the long-term implications of their condition. As a result, they only seek medical attention when their blood pressure becomes dangerously high and starts causing severe symptoms like headaches and dizziness. This delayed approach to managing their chronic disease is common among individuals facing financial constraints. Isolated systolic hypertension was the most common form, affecting almost half of the participants (48.3%). Since the stiffness of the arteries tends to increase with age, systolic blood pressure itself tends to increase with age, resulting in a higher frequency of systolic-type hypertension in the elderly.
This higher prevalence of isolated systolic hypertension in the elderly population can be attributed to the natural ageing process, which leads to a decline in the elasticity of blood vessels. As a result, the systolic blood pressure becomes more prominent and contributes to the development of this form of hypertension.
We observed a strong association between diabetes and hypertension in this study. Specifically, 46.2% of the cases were diabetic, including 33.6% who had been known to be diabetic for between 5 and 10 years. This result is consistent with that published by the national hypertension register, which reported a prevalence of 39%. Hypertension is a shared component of both type 1 and type 2 diabetes. There is strong evidence to support the benefits of reducing blood pressure in people with diabetes to prevent the onset of both the main micro- and macro-vascular complications of diabetes. The proven benefits of blood pressure-lowering treatment in people with diabetes also include a significant reduction in end-stage renal disease, retinopathy, and albuminuria. When considering treatment for hypertension, it is important to ensure that significant orthostatic hypotension, which is likely to occur in diabetics due to the development of autonomic neuropathy, is excluded.
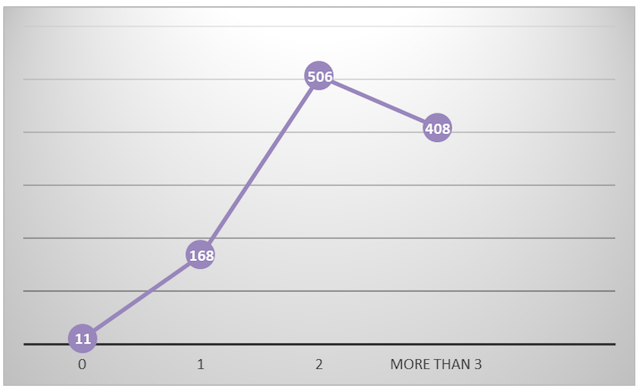
The majority of patients included in the study had two risk factors. 46.3% and 37.3% of them had more than two risk factors, indicating a relationship between different risk factors. It cannot be said that they add up, but rather they potentiate each other. This suggests that the presence of multiple risk factors increases the overall risk level for patients. For example, patients who had both diabetes and obesity were found to have a higher likelihood of developing cardiovascular diseases compared to those with only one risk factor. Therefore, healthcare professionals should consider the combined effect of different risk factors when assessing the health status of their patients and designing appropriate preventive measures.
In this study, 51 patients (4.9% of 1032 cases) were found to have an electrocardiographic abnormality of electrical left ventricular hypertrophy, whereas echographic left ventricular hypertrophy was found in 209 patients (28.7% of 726 cases). The disparity in results between echographic and electrocardiographic data is due to the low sensitivity of electrocardiography in detecting left ventricular hypertrophy despite its good specificity. Although the electrocardiographic method using a multitude of indexes is recommended for the detection of left ventricular hypertrophy, echocardiography remains the gold standard for the detection of left ventricular hypertrophy despite the presence of interpretation biases that depend on the imaging device used and the operator. This means that left ventricular hypertrophy should not be ruled out solely based on the electrocardiogram alone, making echocardiography essential for therapeutic management and follow-up. In addition, the cost of cardiac ultrasound restricts its use, even though several authors believe it to be necessary. A detailed counterexample to the statement would be a scenario where a patient with left ventricular hypertrophy is misdiagnosed and ruled out solely based on the electrocardiogram (ECG) results. Despite the presence of interpretation biases, if the imaging device used and the operator are not able to accurately detect the hypertrophy, it can lead to incorrect diagnosis and subsequent inadequate therapeutic management and follow-up. This highlights the limitations of relying solely on ECG for diagnosing left ventricular hypertrophy.
In our series of patients, we found that left ventricular hypertrophy (LVH) correlates with systolic blood pressure (SBP) values between 100 mmHg and 150 mmHg and not with diastolic blood pressure (DBP), since the majority of cases of LVH (70.3%) occurred at an optimum value of less than 80 mmHg of DBP. The SPRINT trial is therefore aiming for a target SBP of less than 120 mmHg rather than the standard 140 mmHg in order to reduce the risk of cardiovascular complications such as LVH. By lowering the target SBP, the SPRINT trial hopes to further decrease the incidence of LVH and its associated risks. This new approach emphasizes the importance of aggressive blood pressure management in preventing cardiovascular complications and highlights the potential benefits of maintaining SBP values below the traditional threshold.
Coronary artery disease accounts for 40.4% of cases. The epidemiological link between hypertension and ischemic heart disease is very close. According to a register of one million people, hypertension is by far the main cause (43%) of years of life lost due to coronary lesions beyond the age of 30. Any reduction in systolic arterial pressure (SAP) of 10 mmHg reduces the incidence of ischemic heart disease by 17%(15).
The prevalence of atrial fibrillation found in the history of this group of participants was 11.3%, close to that found on the electrocardiogram (10.3%). High blood pressure is conducive to cardiac arrhythmias, including ventricular arrhythmias, but most often atrial fibrillation, which should be considered a consequence of hypertensive heart disease. Even if high blood pressure is normal, it predisposes to the development of atrial fibrillation, and high blood pressure itself is the most prevalent coexisting co-morbidity in patients with atrial fibrillation, which in turn increases the risk of developing stroke and heart failure (16).
Monotherapy accounted for 32.4 percent of the therapeutic regimens in our series, with dual therapy coming in second at 10.8% and triple therapy or more at 4.6%.
This finding aligns with data from Tunisia, where monotherapy is used to treat 48.6% of patients, dual antihypertensive therapy is used for 39.9% of patients, and triple therapy is used for 10.9% of patients.
There is still a role for monotherapy in patients with grade 1 hypertension who are at low cardiovascular risk, despite the fact that multiple authors recommend dual therapy.
In our series, angiotensin-converting enzyme (ACE) inhibitors were prescribed the most frequently (33.4%) among the study participants. Patients on calcium channel blockers (IC) (12.4%), beta blockers (11.9%), and central antihypertensives (12.4%) received the fewest prescriptions. This outcome is explained by the fact that ACE inhibitors are available in the public hospital’s internal pharmacy as well as the fact that the patients in our study were representative of those with diabetes and heart disease, who are the compound’s intended target market.
F. Jarraya et al. report that in 1364 cases (51.2%), a calcium antagonist was the first-line treatment. Converting enzyme inhibitors came in second with 21.9%, b-blockers with 14.6%, and central antihypertensives with 4.7%(20).
With ACE inhibitors and BBs making up 6% of all cases enrolled in our study, this was the most frequently prescribed drug combination. Although it is not the optimal combination in terms of antihypertensive effect (21), beta-blockers in addition to ACE inhibitors are appropriate when the indication exists, particularly in cases of angina, post-infarction, heart failure, rhythm disorders, and left ventricular dysfunction (16).
Secondly, the combination of ACE inhibitor and IC is introduced in 5.3% of patients. This combination is optimal in terms of its antihypertensive effect and is suited to our ageing population, 52% of whom are over 70.
The findings from the ASCOT-CAFE study highlight the superior efficacy of the combination of ACE inhibitors and calcium channel blockers (specifically perindopril and amlodipine) compared to the combination of beta-blockers and diuretics (including atenolol and thiazide) in reducing central systolic blood pressure (cSBP). As a result, our evaluation has prompted a reexamination of the antihypertensive effectiveness of each treatment, with a particular focus on beta-blockers. The diminished efficacy of beta-blockers in safeguarding target organs is attributed to their unfavourable impact on arterial biomechanics (22).
In this study, nearly half of the population studied (49.5%) had an imbalanced blood pressure, with only 50.5% achieving balance through anti-hypertensive therapy. Although these results are better than those reported in the 2005 TAHINA and 2016 THES national surveys, they still fall short of our aims. The TAHINA study found that blood pressure control was achieved in only 24.1% of treated hypertensives, while the THES study reported blood pressure control in only 29.5% of cases (15). These statistics can be partially explained by therapeutic inertia, which tends to result in the prescription of monotherapy rather than dual antihypertensive therapy in the majority of cases. Factors contributing to therapeutic inertia include a lack of knowledge within learned societies, concerns regarding side effects, and inadequate justification for not intensifying treatment, such as focusing solely on a single issue during consultation while disregarding isolated systolic hypertension (23).
Conclusion
More effective approaches to raise consciousness, screening, treatment and management of hypertension are called for in Tunisia overall and in the southern regions of Tunisia more specifically.
Distribution of patients according to age
Distribution of patients according to the number of associated modifiable risk factors
Distribution of Patients with Hypertension by Gender
Table showing the distribution of patients depending on associated comorbidities
|
Associated comorbidities |
Prevalence of patients |
Percentage |
|
diabetes |
505 |
46,2 |
|
Coronary artery disease |
442 |
40,4 |
|
Atrial fibrillation |
124 |
11,3 |
|
Cerebrovascular accident |
56 |
5,1 |
|
Renal failure |
45 |
4,1 |
|
hypothyroidism |
40 |
3,7 |
|
Asthma or chronic obstructive lung disease |
32 |
2,9 |
|
Suspected sleep apnoea syndrome |
13 |
1,2 |
|
Confirmed sleep apnoea syndrome |
4 |
0,4 |
Classification of patients based on the management of their blood pressure
Table showing the different combinations of treatments available
|
Drug combinations |
Prevalence of patients |
Percentage |
|
IEC + BB |
66 |
6 |
|
AEC inhibitor + IC |
59 |
5,4 |
|
IC + BB |
34 |
3,1 |
|
AEC inhibitor + diuretic |
33 |
3 |
|
ARBs + IC |
26 |
2,4 |
|
IC + diuretic |
18 |
1,6 |
|
BB + diuretic |
18 |
1,6 |
|
ARBs + diuretic |
14 |
1,3 |
|
ARBs + BB |
7 |
0,6 |